‘ACTING OUT’ BEHAVIOUR OF TRAUMATIZED CHILDREN, THROUGH THE LENS OF POLYVAGAL THEORY – PATRICK TOMLINSON (2019, revised 2025)
Date added: 18/02/22
Download a Free PDF of this Article
Recently I have been learning, or trying to learn might be more accurate, about polyvagal theory. I am thinking about its application to work with traumatized children and young people. Although, what I have understood so far is relevant in many other areas of life and work. I have been reading Stephen Porges (2017) – The Pocket Guide to the Polyvagal Theory: The Transformative Power of Feeling Safe. Like the 2nd part of the title implies, this is fundamental to working with trauma, and hence my interest. If the title of Porges’ book suggests easy reading, I would say it is not, but it is written clearly, and I am finding it very helpful.
Learning a new theory is always a challenge, but when a theory is connected to our own experience it is easier to conceptualize. It also helps us when a new theory fits well on top of other theories, which we already understand well. Development is usually incremental. I believe in the practical implications and use of theory. As Kurt Lewin (1943) a pioneer in organizational psychology famously noted, there is nothing so practical as a good theory. Tongues (2016, p.80) succinctly states the usefulness of a good theory,
A theory is an explanation, a set of ideas about how something works, and the practical application of good theory can be invaluable.
The polyvagal theory is especially useful in helping us understand some complex issues. So, I am going to try and apply it to something I have been talking about recently – the meaning of ‘acting out’ behaviour of children who have suffered complex trauma. In particular, the phenomena of ‘running away’ behaviour, which I wrote about in a previous blog (Tomlinson, 2015a).
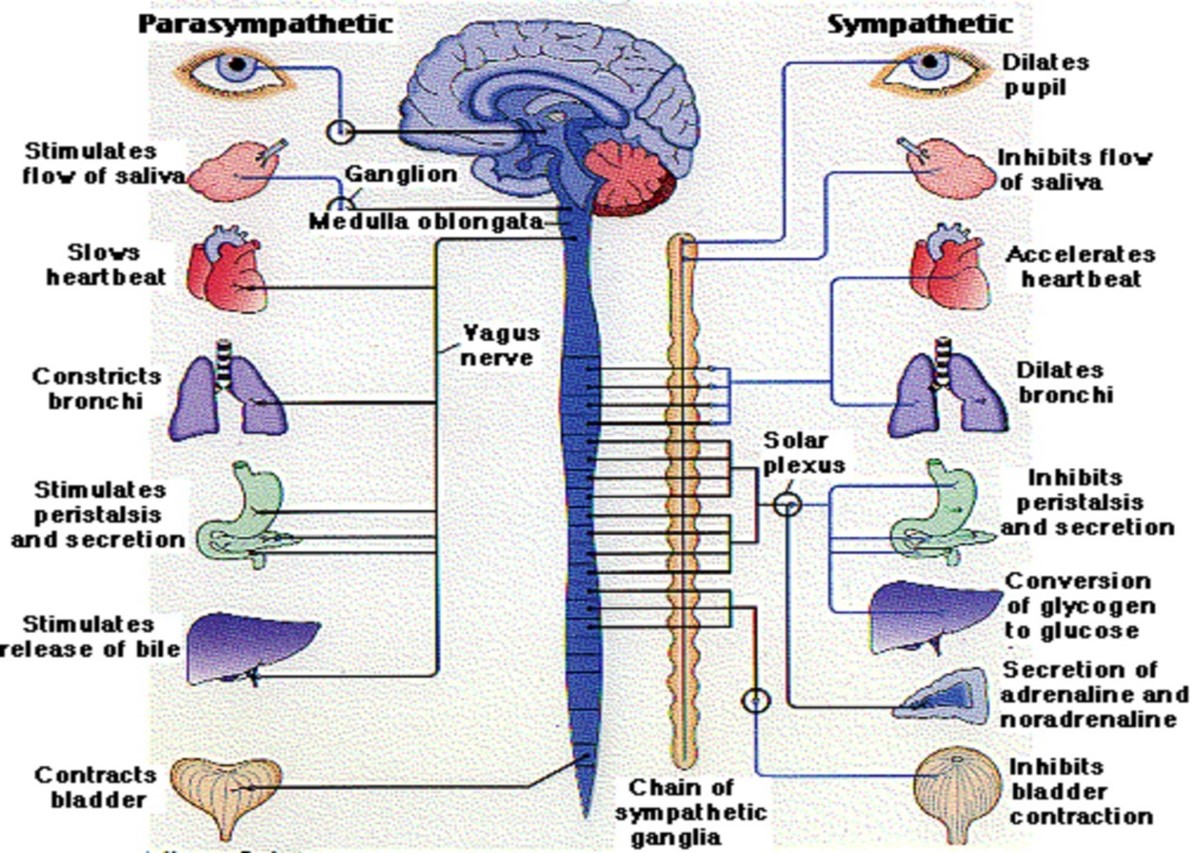
 Porges explains that a vagal pathway (nerve) is part of the autonomic nervous system and poly means there are many of them. The vagal pathways function to protect safety. They alert the person to threat and mobilize a protective response. This happens at an unconscious level, which Porges refers to as neuroception. In other words, it is the nervous system that is identifying threats to safety, as well as opportunities for enhancing safety and well-being. Dana (2018, p.35 ) summarizes,
Porges explains that a vagal pathway (nerve) is part of the autonomic nervous system and poly means there are many of them. The vagal pathways function to protect safety. They alert the person to threat and mobilize a protective response. This happens at an unconscious level, which Porges refers to as neuroception. In other words, it is the nervous system that is identifying threats to safety, as well as opportunities for enhancing safety and well-being. Dana (2018, p.35 ) summarizes,
“Neuroception results in the gut feelings, the heart-informed feelings, the implicit feelings that move us along the continuum between safety and survival response. Neuroception might be thought of as ‘somatic signals that influence decision making and behavioural responses without explicit awareness of the provoking cues’ (Klarer et al., 2014, p.7067).”
When we are in danger neuroception takes charge and overrides our thought processes. I experienced a vivid demonstration of this. I was on a beach in Israel where a group of soldiers had set up a temporary camp. Suddenly, I heard a loud bang behind me. Before I knew it, I was sprinting and ended up about 30 yards down the beach. I was safely in the sea before I stopped to turn around. Thankfully, no one was injured. There had only been a minor explosion of a cooking gas canister and nothing more sinister. I remember wondering how I moved so quickly and so far without even thinking. Good job my neuroception was working well and gave the orders to flee! Problems arise when the vagal pathways have been impacted by trauma, especially of the complex kind. Neuroception becomes hypervigilant, misreads situations and may respond to safe situations as if they are dangerous. We know this well in our work with trauma.
Theoretical understanding of the centrality of safety in healthy development and treatment is not new. Bowlby (1952, 1988) explained the concept of how a secure base is the starting point of healthy development during infancy. In the treatment of trauma, Pierre Janet in the 19th century outlined that safety/stabilization was the first phase of treatment followed by processing and integration (Kezelman and Stavropoulos, 2012, p.17). In work with traumatized children and others, safety is the starting point. The child must actually be safe and then reach the point where he/she also feels safe. Feeling safe is not the same as being safe. It might take a year or longer of being safe before he/she begins to feel safe. And there will be plenty of ups and downs along the way. Before connections can be achieved, safety must be established. Only when a disconnected or unconnected child begins to feel safe will he/she be able to take the risks involved in connecting. Once the process of connecting begins the child is moving towards integration.
The foundations of well-being can be considered as safety, connection and integration (Tomlinson, 2015a).
A brief look at Porges’ breakdown of the autonomic nervous system, into three distinct functions helps elaborate our understanding of safety. The oldest part of the nervous system is the dorsal vagal circuit, which developed over 500 million years ago. It can be considered reptilian. This is part of the parasympathetic nervous system. The dorsal vagus takes hold when a person feels trapped and in life-threatening danger. The typical responses include freezing, becoming immobile, fainting and appearing dead. The aim is to be still, to avoid an attack. And if attacked the heart rate and breathing are slowed, blood is withdrawn from the surface of the body to the organs. This is a survival, energy-conserving response that makes death less likely if attacked and injured.
Another feature of the dorsal vagal circuit is dissociation. This is where the person who is physically trapped in a traumatic situation becomes psychically removed from their body. Again, this is not a conscious process. Sometimes afterwards a person talks about being outside of their body, observing what was happening but not feeling the pain. It is also possible that they may have no conscious memory of the event. Dissociation is a protective function, but if repeated regularly it can begin to have serious consequences for healthy functioning. As Van der Kolk and Newman (2007, p.7) state,
…posttraumatic syndrome is the result of a failure of time to heal all wounds. The memory of the trauma is not integrated and accepted as a part of one's personal past; instead, it comes to exist independently of previous schemata (i.e., it is dissociated).
I was fortunate to begin my work at the Cotswold Community, a therapeutic community in England. It was for boys who had suffered complex trauma. The therapeutic approach was based on the work of Psychoanalyst and Pediatrician, Donald Winnicott. Our consultant Barbara Dockar-Drysdale (1958) had developed the concept of a ‘frozen’ child. This was one of the syndromes of deprivation (1970, 1970a), that children developed as defence mechanisms in response to repeated trauma, including neglect and abuse. A ‘frozen’ child usually had the most serious levels of abuse and neglect often from birth. I think the frozen child had much in common with a child whose dorsal vagal circuit is hypervigilant. Dockar-Drysdale (1958, p.17) explained her preference for the term ‘frozen’ rather than ‘affectionless’, which was also used at the time, because,
… ’affectionless’ sounds final, but a thaw can follow a frost.
A thaw of something frozen inevitably means movement. This progression can also be linked to the second part of our autonomic nervous system, which developed 400 million years ago. This is the sympathetic nervous system and is mobilized in response to danger. As in a thaw, mobilization means movement and is a progression from the freezing function of the dorsal vagal circuit. The sympathetic nervous system prepares our body for action. Faced with danger this is in the form of fight/flight.
 Accurate neuroception detects a threat from which there is a possibility of escape, as in my experience on the beach. Where neuroception is over-active, as is often the case with traumatized children, danger may be perceived where there is none, or the level of it is exaggerated. So, the child over-reacts, and fights or takes flight when there is no actual need. This can happen very quickly from a state of apparent calm and is often bewildering to those involved. However, we might all recognize our own ‘trigger’ points, which can lead to defensive over-reactions. (pic, Anxiety Canada, 2019)
Accurate neuroception detects a threat from which there is a possibility of escape, as in my experience on the beach. Where neuroception is over-active, as is often the case with traumatized children, danger may be perceived where there is none, or the level of it is exaggerated. So, the child over-reacts, and fights or takes flight when there is no actual need. This can happen very quickly from a state of apparent calm and is often bewildering to those involved. However, we might all recognize our own ‘trigger’ points, which can lead to defensive over-reactions. (pic, Anxiety Canada, 2019)
Thinking of this about running away, there may be different things going on. The child who runs away may be in a fearful state and has sensed a threat, whether it exists or not. The aim is to escape. Another child in the same situation may perceive the threat to be even more serious, and he or she may freeze rather than flee. The dorsal vagal circuit for this child may be dominant and the first form of defence.
For anyone working with this, such as a carer, the fleeing child may evoke more anxiety than the freezing child, though the fleeing child may be healthier and less traumatized. This reminds me of Winnicott’s (1956, 1967) concept of the antisocial tendency and delinquency as a sign of hope. The fighting/fleeing child is at least ‘alive’ and mobile. The nuisance caused by the child also contains hope, which provides an opportunity for us to respond and nourish. Children who have suffered inescapable terrifying abuse, often feel that their bodies are useless and a source of shame. It seems a natural and healthy consequence in the process of recovery that the ability to escape might be put to the test. Feeling that this is now possible can be seen as a hopeful development.
Clearly, we don’t want traumatized children running away just to prove that they can. There is also always the possibility that the situation is not so benign and something real is causing fear. We always need to be vigilantly aware of any possibility of abuse or potential harm. Establishing and preserving safety is always the number one priority. We should make sure that the environments we provide for children are nurturing and emotionally containing. Early in my therapeutic community career as a part of our training we watched a video of the psychologist, Bruno Bettleheim (1986, Part 2, 5.58), talking about his pioneering work in the Orthogenic School in Chicago, explained that sometimes a child could not be stopped from running away so rather than ‘run after him’ they tried to ‘run with him’.
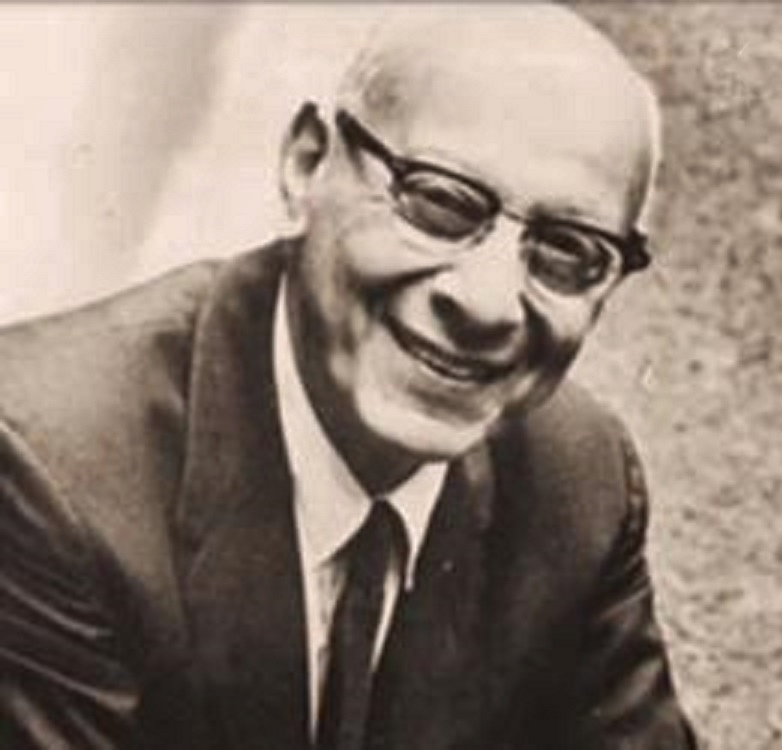 “One of the changes I made when I took over the school was to change all the locks and do away with all the keys. Because when I took over every door had a lock, and the children could be locked in. I thought this was an abomination. So, I took all the locks of all the doors inside the institution and so locks were only against the outside. The entrance doors could be locked against the outside but not against the inside. So, any child who wanted to run away could run away – which in short did away with most running away. Now there were always some children at their beginning who had to run. What we tried to do was have a staff member run with them and accompany them, but not run after them, because to run after a child is very risky. He might run out in the street in front of an oncoming car. So, when we run with the child, we had to be very clear it was to keep him company wherever he wanted to go and to protect him against all dangers in the running away. But not to bring him back or force him back.”
“One of the changes I made when I took over the school was to change all the locks and do away with all the keys. Because when I took over every door had a lock, and the children could be locked in. I thought this was an abomination. So, I took all the locks of all the doors inside the institution and so locks were only against the outside. The entrance doors could be locked against the outside but not against the inside. So, any child who wanted to run away could run away – which in short did away with most running away. Now there were always some children at their beginning who had to run. What we tried to do was have a staff member run with them and accompany them, but not run after them, because to run after a child is very risky. He might run out in the street in front of an oncoming car. So, when we run with the child, we had to be very clear it was to keep him company wherever he wanted to go and to protect him against all dangers in the running away. But not to bring him back or force him back.”
At the time, I found this an insightful way of re-framing the problem. Maybe sometimes our job wasn’t to stop a child from running away but to make the running away safe. To be alongside the child. There may be other things we can do to help improve safety. For example, if we think that a young person is likely to run away, we can make sure that he has useful phone numbers he can use if he needs help. According to Streitfeld (1990) Bettleheim could also identify with the truant mind. Or when a child was found to be skipping school, instead of chastising him, Bettelheim admitted: "If I had the courage, I would have skipped school too. The only problem was, I wasn't brave enough. He must have a good reason for not wanting to go. I wonder what it is."
The point wasn't to excuse; it was to understand. Bettleheim’s approach was well before polyvagal theory. However, we can see how much there is in common. The fearful child is taking flight, As Porges says, the sympathetic nervous system is mobilized. Bettleheim recognizes that chasing after the child only to bring him back is likely to add to the child’s fear. So, Bettleheim suggests running with the child to help him be safe. This is more likely to have a calming fact. The child may still be running but now the mobilization can be used socially rather than to escape. The sympathetic nervous system can potentially be used healthily as a protective factor.
We can also help the young person use movement and gain a sense of physical competence in many other ways. For example, playing sports, bike riding, running, skipping, music and dancing. Games such as tag and, hide and seek, which allow a feeling of being able to escape might also provide an excellent way of fostering a newfound sense of belief in a competent body. We can see that as Porges says, the mobilization of the sympathetic nervous system, can be playful and not just fight/flight. Simon Bain (2012), a resident of the Cotswold Community in the 1970s, seems to suggest this when he talks of his memories of running away,
Although, you could say, I wasn’t a success - the funniest and indeed my fondest memories are the ‘running outs’ we used to do, with the staff spending half the night chasing us.
Porges (2017, p.129) states,
The difference between the fight/flight and play is that while mobilizing, we’re making eye contact and engaging each other. We’re diffusing the cues of threat with social cues, so we can utilize the sympathetic nervous system to support movement without moving into defensive fight/flight behaviours. When we involve the social engagement system, we can even use the oldest system, which is immobilization, and we can be in the arms of someone that we feel safe with.
The final and most recently evolved part of the autonomic nervous system is the ventral circuit. As with the dorsal vagus, this is part of the parasympathetic nervous system. It evolved 200 million years ago and is uniquely mammalian. The ventral circuit looks for safety and social connection. In this sense, it could be considered as a preventative and anticipatory part of the nervous system. It gives us the capacity to co-regulate (Dana, 2018). The neuroception involved is picking up cues for connections that will add to our safety and hence improve our potential for survival. Unfortunately for many traumatized children this function of the nervous system is shut down and underdeveloped.
Conditions of safety and repeated positive experiences are essential for it to develop and come into use. This will happen as the dorsal vagus and sympathetic circuits are less active. As freeze, fight/flight are reduced, moments of calm are increasingly possible. Connection is a hugely protective factor that promotes further development. Once connections are established potential threats are reduced. As Porges (2017, p.43) explains this important aspect of polyvagal theory,
 “Moreover, and perhaps most important, the theory explains how safety is not the removal of threat and that feeling safe is dependent on unique cues in the environment and our relationships that have an active inhibition on defense circuits and promote health and feelings of love and trust (e.g., Porges, 1998).”
“Moreover, and perhaps most important, the theory explains how safety is not the removal of threat and that feeling safe is dependent on unique cues in the environment and our relationships that have an active inhibition on defense circuits and promote health and feelings of love and trust (e.g., Porges, 1998).”
Once protective connections are established, these can be used to anticipate and prevent the activation of the dorsal vagal and sympathetic circuits. Once this begins the individual is more in the connecting and less in the defensive state. This begins a positive spiral where the person is on the road to recovery. Acting out, such as running away are now less likely.
I have outlined how the three parts of the autonomic nervous system may be activated and their use in promoting our safety, survival and well-being. Understanding the different functions is vital to effective treatment. For example, the sympathetic circuit of fight/flight, whilst being more difficult to manage may mean the child is in a healthier state than if he/she was freezing and immobile.
Using running away as an example, not running may be at both ends of the spectrum of frozen and connected. Stillness can be due to calm safety or fear. The difference between the two can be sensed by our neuroception – how we unconsciously read and are attuned to what is happening. The difficult job of responding to running away behaviour offers the potential bridge between the dorsal vagal and ventral circuits. The fight/flight and playful mobilization of the sympathetic nervous system, however challenging may also contain the hope that Winnicott referred to over fifty years ago.
As Porges (2017, p.56) states,
I want to emphasize that understanding the response, not the traumatic event, is critical to the successful treatment of trauma.
References
Bain, S. (2102) Comment posted on John Whitwell: A Personal Site of Professional Interest, www.johnwhitwell.co.uk
Bettleheim, B. (1986) Documentary Horizon Part 1 - https://www.youtube.com/watch?v=IEi7QVtk-Ms&t=23s Part 2 - https://www.dailymotion.com/video/x7n0igf
Bowlby, J. (1951) Maternal Care and Mental Health, WHO Monograph 2, Geneva: World Health Organization
Bowlby, J. (1988) A secure base: Parent-child attachment and healthy human development, New York: Basic Books
Dana, D. (2018) The Polyvagal Theory in Therapy: Engaging the Rhythm of Regulation, New York and London: W.W. Norton and Company
Dockar-Drysdale, B. (1958) The Residential Treatment of ‘Frozen’ Children, in Therapy and Consultation in Child Care (1993), London: Free Association Books
Dockar-Drysdale, B. (1970) Syndrome, in Therapy and Consultation in Child Care (1993), London: Free Association Books
Dockar-Drysdale, B. (1970a) Need Assessment – 11, Making an Assessment, in Therapy and Consultation in Child Care (1993), London: Free Association Books
Kezelman, C. and Stavropoulos, P. (2012) The Last Frontier: Practice Guidelines for Treatment of Complex Trauma and Trauma Informed Care and Service Delivery, Australia: Adults Surviving Child Abuse (ASCA), http://goo.gl/t9o3lA
Klarer, M., Arnold, M., Guther, l., Winter, C., Langhans, W. and Meyer, U. (2014) Gut Vagal afferents Differentiately Modulate Innate Anxiety and Learned Fear, in Journal of Neuroscience, 34(21) pp.7067-7076
Lewin, K. (1943). Psychology and the process of group living. Journal of Social Psychology, 17, 113–131. Reprinted in, The complete social scientist: A Kurt Lewin reader, (Gold, Martin, Ed) (1999) (pp. 333–345). Reprinted (in part) in Cartwright, 1951, Chapter 7
Porges, S.W. (1998) Love: An Emergent Property of the Mammalian Autonomic Nervous System, in Psychoneuroendocrinology, 23(8). 837--861
Porges, S.W. (2017) The Pocket Guide to the Polyvagal Theory: The Transformative Power of Feeling Safe, New York and London: W.W. Norton and Company
Tomlinson, P. (2015) Integration and Connection in Well-Being and Recovery from Trauma
www.linkedin.com/pulse/integration-connection-well-being-recovery-from-trauma-tomlinson
Tomlinson, P. (2015a) Reasons a Traumatized Child Runs Away? www.linkedin.com/pulse/reasons-traumatized-child-runs-away-patrick-tomlinson
Tonges, M.C. (2016) Nothing so Practical as a Good theory, in Nurse Leader, February 2016, Vol. 14, Issue 1, www.nurseleader.com/article/S1541-4612(15)00297-9/abstract
Vagus Nerve Diagram (2011) Seng Nduwe Ngamuk http://sengnduwengamuk.blogspot.com/2011/02/vagus-nerve-diagram.html
Van der Kolk, B.A. and Newman, A.C. (2007) The Black Hole of Trauma, in van der Kolk, B. A., McFarlane, A. C. and Weisaeth, L. (eds.) Traumatic Stress: The Effects of Overwhelming Experience on Mind, Body and Society, New York: Guilford Press
Winnicott, D.W. (1956) The Antisocial Tendency, in D.W. Winnicott (1984) Deprivation and Delinquency, London and New York: Tavistock Publications
Winnicott, D.W. (1967) Delinquency as a Sign of Hope, A talk given to the Borstal Assistant Governors’ Conference, held at King Alfred’s College, Winchester, April 1967, retrieved from
https://www.johnwhitwell.co.uk/child-care-general-archive/delinquency-as-a-sign-of-hope/
Files
Please leave a comment
Next Steps - If you have a question please use the button below. If you would like to find out more
or discuss a particular requirement with Patrick, please book a free exploratory meeting
Ask a question or
Book a free meeting













